PhilHealth
home | contact us | sitemap | disclaimer
News
PhilHealth Delegation Joins Experts’ Meet for DRG Development and Reforms October 17, 2018
HO CHI MINH, VIETNAM –Thirty-three (33) government officials, consultants, and experts from Vietnam, Thailand, Malaysia, Indonesia, and the Philippines gathered here recently at the Pullman Saigon Centre for their first meeting to advance a Diagnosis-Related Group (DRG)-based health care provider payment system in Southeast Asia. The activity was organized by the World Bank (WB).
The event featured DRG specialists and health administrators from the participating countries. Economic experts of the WB and the United States Agency for International Development (USAID) were also present, together with authorities of the Nordic Case Mix Center, which coordinates the maintenance, updating, and further development of the NordDRG system of provider payment in countries such as Finland, Norway, Sweden, Denmark, Iceland, Estonia, and Latvia.
Dr. Roy B. Ferrer, Acting President and Chief Executive Officer of the Philippine Health Insurance Corporation (PhilHealth) led the delegation of the state social health insurer. He was joined by Dr. Roberto Salvador, representative of the Formal Sector in the PhilHealth Board of Directors, Dr. Melanie Santillan, Officer-in-charge-Senior Manager of the Benefits Development and Research Department; Maja Riel of the Office of the Executive Vice President and Chief Operating Officer, and the author representing the Corporate Communication Department. The Philippine Department of Health (DoH) was represented by Assistant Secretary Dr. Lyndon Lee Suy and Dr. Maria Iris Baltazar, Medical Officer III.
“This [meeting] presents PhilHealth with an opportunity to learn from our neighboring countries. A lot can be taken from their experiences in the implementation of a DRG-based payment for services rendered by health care providers,” said Ferrer. “We shall be able to compare our current system with that of the standards of DRG and decide on the best course of action to improve our claims reimbursement procedures. It could also help us enhance our benefits and services.”
Vietnam Vice Minister for Health Pham Le Tuan formally welcomed the participants saying that, “This workshop could potentially be the starting point of an on-going collaboration between participating countries in DRG development and reform.” He added that Vietnam had deployed pilot implementations of the DRG in some of their hospitals. Tuan also acknowledged Thailand’s support in improving their diagnosis classification system.
Caryn Bredenkamp, WB Senior Health Economist, believed that a lot can be gained from sharing experiences, challenges, and knowledge, even as she encouraged consistent collaborations in the future with the end-view of attaining progress in the region-wide DRG operations.
“From a technical efficiency standpoint, DRGs are considered the best payment model,” observed Jack Langenbrunner, a USAID health economist. “It facilitates competition between providers, improves responsiveness to patient needs and enhances cost transparency and efficiency within providers.”
The DRG-based payment is a fixed amount per case of a given case type – DRG –wherein the amount for a given case type is determined by its relative cost weight while other elements such as base rate and adjustment factors affect the computation outcome in this set-up.
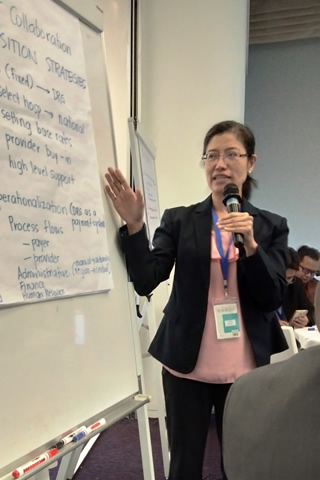
During her presentation, Santillan detailed PhilHealth’s journey on provider payment reforms from the fee-for-service era to shifting to all case rates and towards transitioning to a more responsive provider payment mechanism. The Philippines remains the only country in the region that has yet to adopt the DRG system.
Two crucial policy reforms on provider payment are in order for the National Health Insurance Program (NHIP) that shall support attainment of Universal Health Coverage and achievement of financial risk protection. The first is transitioning the current case rates payment system for inpatient services to a DRG-based Global Budget payment system, while maintaining the outlier high cost services by the Z Benefits and expanding the primary care benefits to all. Second is to establish co-pay limit, “Delivering true financial protection requires coordinated policies for both patients and providers,” Santillan maintained. “For the vulnerable and marginalized population, we intend to fully implement the No Balance Billing (NBB) policy for basic services and accommodation, while for the non-vulnerable population; out of pocket expenses should be regulated by a co-pay ceiling.” On the part of health care providers, Santillan mentioned that PhilHealth “...with proper costing of health care services, providers would receive appropriate and fair incentives for the services that they deliver.”
In a separate presentation, Baltazar detailed the efforts being undertaken by the Philippine health sector to progress the development of a DRG provider payment system. She cited meaningful collaborations with development partners –the European Union (EU), Thailand, and the WB.
“The EU provided valuable assistance in designing a 5-year road map that laid out the elaborate steps needed to shift towards a DRG payment system. In addition, the Union had contributed in building an organizational structure and identifying human resource requirements to meet the demands of the transition,” Baltazar revealed.
On the other hand, Thailand was chosen to share its expertise to simulate Philippine data using the Thai DRG grouper system. A grouper is a software package that assigns a DRG specific to the patient’s episode of care. The grouper uses data that reflects the principal diagnosis and comorbidities coded in the International Classification of Diseases (ICD) classification, age, sex, surgical procedures, and length of stay and other relevant information that would then become the basis of payment to health care providers.
As to the collaboration with the WB, Baltazar said, “The World Bank is willing to validate the implications of adopting the Thai DRG or another existing grouper. They will also help us do an in-depth review of the All Case [Rates] system. We need hard evidence on the quantitative and qualitative aspects of the All Case Rates to encourage our policy-makers to shift [to DRG].”
The participating countries recognized their own shortcomings in implementing a DRG-driven provider payment method. A prominent challenge was developing a grouper system that effectively catalogues medical conditions and surgical procedures. Some of the factors affecting system development were data gathering and coding standards. Other challenges such as transitional strategies and operational application also came into play.
Triin Habicht, a health financing and DRG expert from Estonia, offered ways to successfully manage risks associated with the employment of DRG. She pointed out that a timely monitoring system must be used to detect unexpected practices and, in turn, pave the way for necessary adjustments. Habicht was adamant on the quality of DRG coding and insisted that the participants must conduct trainings, streamline guidelines, and strengthen controls for preferred outcomes.
Payment adjustments, budget ceilings, and aligned payment incentives across different care settings were among her recommendations to influence the attainment of a DRG-based payment scheme in the region.
Transitioning to another method of health care purchasing system is already a daunting task for PhilHealth and the DoH, let alone the rest of Southeast Asia. Impossible, some would say. Unmanageable, some would agree.
What occurred here was a collective show of support to an agenda which aims to ward off financial exhaustion during medical predicaments. The employment of a DRG payment mechanism is a huge step towards Universal Health Care as it promotes a highly-effective and sustainable approach to health care financing. The DRG guarantees fair costs on the part of the insurer and appropriate incentives to health care providers; serving the best interests of everyone involved in caring for the sick.
Ultimately, policy makers play a huge role in securing the success of this endeavor. Achievement of desired results will prove difficult without the support of each nation’s government and might result to a delay in the implementation of a payment standard that can potentially become the benchmark of social health care excellence.
As the meeting closed, the participants decided to have a continued collaboration among themselves in an effort to keep tabs on each other’s progress and afford assistance to those in need, thereby forming an allegiance committed to propel a health care financing built upon the principles of DRG into realization.
Plans were hatched, partnerships were forged, and progress was promised at the conclusion of such productive convention. Finally, the group agreed to a succeeding meeting. In the Philippines, maybe? Let’s see. (END) (JJ Rico)