PhilHealth
home | contact us | disclaimer
News
PhilHealth conducts multi-sectoral anti-fraud fora May 6, 2013
THE Philippine Health Insurance Corporation (PhilHealth) recently orients other government agencies, non-government organizations, members of the Philippine Hospital Association and accredited collecting partners in General Santos City on the significance of its anti-fraud program to ensure continuous provisions of quality health care services to all its members.
The Fact Finding Investigation and Enforcement Department (FFIED) of PhilHealth presented to the participants their fraud prevention and control programs, such as the 'Oplan Kisapmata' which monitors claims benefits and utilizations on cataract surgery performed during medical missions and thru recruitment schemes. The FFIED also presented the important roles being handled by the accreditation and quality assurance and legal services Office on the anti-fraud campaign in the regional level to curb-out, if not totally eradicate fraud practices being committed by some erring healthcare providers.
PhilHealth Vice President for Area IV Ramon F. Aristoza pointed out some problems on fraud related to healthcare that are prevalent still, which include padding of claims or making it appear that the member is confined beyond the actual days of illness; claims for non-admitted patients; extending period of confinements; post dating of claims; misrepresentation by filing false or incorrect information; filing of multiple claims; unjustified bed capacity; fabrication of forms and other fraudulent acts.
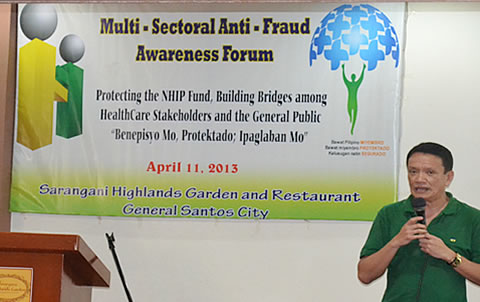
Photo shows Atty. Alexander A. Padilla, PhilHealth Executive Vice President and Chief Operating Officer, during the Q&A session on fraud prevention where he stressed that PhilHealth is financially capable and very generous in terms of paying the hospitals provided that they render the necessary services needed by its members. (END)